The Candida Syndrome: Health Nemesis or Myth?
by Charles W. Moore
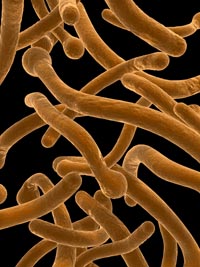
Photo © Sebastian Kaulitzki/Shutterstock |
Candida albicans is a yeast-like fungal parasite inhabiting the digestive tracts of nearly all adult humans. Normally, Candida peacefully co-exists with other microbial passengers in our bodies. However, it also appears to be a cause of a wide variety of disorders ranging from bad breath to serious neurological disorders. It’s also controversial – at least among the mainstream medical community.
Candida albicans infections are one of the major health problems of our era. Some doctors claim that 60 to 80 percent of the population may be affected. Others dismiss alleged chronic Candidiasis as the cause of a variety of seemingly unrelated disease symptoms as merely the latest fad diagnosis. One reference I consulted describes what it calls the “Candida Syndrome” as a “mythical disease.”
On the other hand, authors such as, C. Orian Truss in The Missing Diagnosis II, William Crook in The Yeast Connection: A Medical Breakthrough and Keith Sehnert in The Candidiasis Syndrome, assert that Candidiasis can cause or mimic virtually any disease symptom from bad breath to Multiple Sclerosis-type neurological disorders. A partial inventory of claimed Candida-related symptoms includes: difficulty concentrating (“brain fog”), slowed reflexes, depression, lethargy and apathy, decreased mental energy, anxiety, fatigue, obsessive-compulsive disorder, PMS and breast swelling/tenderness in women, headaches, memory loss, hives, seborrhea, psoriasis, skin rashes, diarrhea, constipation, bloating, nasal congestion, sinusitis, infertility, ocular “floaters,” prostatitis, pelvic pain, loss of libido, neuritis, arthritis, Crohn’s disease, hypoglycemia, schizophrenia, anorexia nervosa, lupus, hyperactivity, behavior and learning problems and autism.
Such claims scandalize many conventional M.D.s, who were taught in medical school that particular symptoms relate diagnostically to specific disorders. “Most traditional doctors do not want to hear about this condition and call it a ‘fad’ disease,” says Candida researcher Elson M. Haas, M.D. “However, with long-term infestation or with the weakened immune state that can result from a reduction of normal colon bacteria, the yeast can shift into its fungal form, wherein it develops rhizoids, or roots, that can be implanted in the intestinal wall or other mucosal linings.”
Candida albicans is a yeast-like fungal parasite inhabiting the digestive tracts of nearly all adult humans. Normally, Candida peacefully co-exists with sundry other microbial passengers in our bodies. Because it is so ubiquitous, a positive test for Candida’s presence is not very useful as a diagnostic tool. Routine blood tests usually don’t reveal anything unusual.
Candidiasis is a “respectable” medical diagnosis within a limited scope. Thrush – a Candida infection of the mouth and throat – is acknowledged by the medical establishment, as is vaginal Candidiasis in women. It is attribution of less specific ailments to Candida that is controversial. Many physicians recall being told in medical school that Candidiasis affects only the severely immunosuppressed.
If Candidiasis is as rampant as some suggest, what is the cause? Several explanations are postulated:
1. Massive overprescription and misuse of antibiotics and steroid drugs in medicine and agriculture is cited. Antibiotics ingested as medication or from residues in meat and dairy products are powerless against yeasts, but destroy “friendly” bacterial gut inhabitants, making room for opportunistic Candida to grow. Friendly bacteria don’t just “crowd out” intestinal yeast, but also produce factors such as lactic acid, formic acid, acetic acid, and hydrogen peroxide that help create an environment unfavorable to yeast. Oral contraceptive drugs and anti-ulcer medications (Tagamet, Zantac, Pepcid, Axid) are also identified as having a probable role in promoting Candida overgrowth.
2. It is suggested that allegedly “sub-toxic” concentrations of synthetic chemical pollutants that virtually everyone in the developed world is exposed to 24 hours a day – in homes, workplaces, public buildings, and outdoor air – are stressing our immune systems to a degree that they can’t cope with aggressive and persistent parasites like Candida.
| Candida albicans infections are one of the major health problems of our era. Some doctors claim that 60 to 80 percent of the population may be affected. |
3. It is further theorized that mercury amalgam (“silver”) dental fillings slowly poison the immune system and encourage Candida growth. Candida have the unusual ability to interact with the toxic metal mercury, and are believed by some to proliferate when there is more mercury in the body. “When the body’s burden of mercury is low and the normal intestinal germs are present, Candida does not grow excessively and the body feels well,” says Gordon Josephs, M.D.
4. It is also believed that our society’s high dietary consumption of sugar and other simple carbohydrates, and generally low consumption of high fiber complex carbohydrate foods creates ideal body chemistry for Candida overgrowth. Simple sugars are rapidly metabolized by yeasts/fungi, and also inhibit friendly bacteria growth.
5. Candida produces 79 distinct toxins, that allegedly cause a broad range of symptoms, which tend to become chronic because the toxins also adversely affect the immune system, facilitating continued Candida growth and toxin production. “Candida is responsible for flooding the system with an accumulation of toxic acetylaldehydes. Acetylaldehydes are known to poison tissues – accumulating in the brain, spinal cord, joints, muscles and tissues.” says Dr. Stephan Cooter, Ph.D, in his book Beating Chronic Disease.
6. Candida has also been suggested to play a part in creating what is called a “leaky gut.” Fungal Candida roots in intestinal walls, perforating them microscopically and allowing undigested food particles and fecal matter to pass directly into the bloodstream. This swamps the immune system and triggers a sensitizing response to normally harmless molecules. The individual becomes “environmentally sensitive,” reacting to normally harmless inhalants in the environment. Increased stress on the immune system further weakens the body’s ability to fight Candida, and a vicious cycle is established. Fugitive particles from the gut may also pass through the blood/brain barrier, be mistaken for neurotransmitters, and produce mental and neurological symptoms.
Nonsense, says the Infectious Diseases and Immunization Committee of the Canadian Paediatric Society, in a paper intended to debunk popular “misconceptions” about the Candida Syndrome, which the report characterizes as “a concoction of a few truths and many unproven assertions.” The authors continue: “Although the increase in Candida colonization associated with the use of antibiotics, particularly broad-spectrum ones, is well established, there is no proof that this results in the production of Candida toxins....– the hypothesis of ‘chronic candidiasis’ must be considered speculative and unproven.”
The report also notes that “The symptoms reportedly caused by ‘chronic candidiasis’ are so varied and general that nearly every person could have them at one time or another.” However Candida Syndrome proponents argue that it is precisely the presence of multiple symptoms that may be an indicator of Candidiasis. Indeed, symptoms like headaches, allergic disorders, depression, panic attacks, irritability, and anxiety, are believed to be typical consequences of the effect of Candida-toxins on brain chemistry.
Even when a diagnosis of Candidiasis is affirmed, treatment is nearly as controversial as the disease itself. There are three basic modes of Candidiasis therapy:
1. Pharmaceutical anti-fungal drugs like Nystatin, Ketoconazol, Monistat, Lamisil (Terbinafine HCl), Diflucan (Fluconazole), Sporanox (Itraconazole), etc. Lamisil is a new fungistatic (stops growth of fungi) and fungicidal (kills fungi) which may replace Diflucan as the drug of choice for treating Candidiasis. Nystatin is the weakest antifungal and many yeast are resistant to it.
2. Naturopathic or nutraceutical anti-Candida dietary supplements such as garlic, Caprylic Acid, Black Walnut, Olive oil, Psyllium husk and seed powder, Pau d’Arco, Molybdenum, Deglycyrrhizinated Licorice (DGL), Glucosamine and N-acetylglucosamine (NAG), Concanavolin A, Manapol, Undecylenic acid, Gentian violet, digestive enzyme supplements, and various homeopathic formulas, among others.
3. A combination of the two above approaches.
Most Candida therapists recommend diets restricted in sugars, other simple carbohydrates and alcohol, as well as avoiding antibiotics (topical and oral), hormonal, cortisone (steroid), and antacid/anti-ulcer medications. Neither anti-fungal drugs nor Naturopathic anti-fungals can work successfully without removing sugars from the diet, including all sweetened drinks, soda pop, fruits and fruit drinks, and corn syrups. Candida ferments and proliferates in the presence of simple sugars. Sugar dramatically increases Candida’s ability to stick to mucus membrane cells.
Avoid non-essential antibiotic medications as well as antibacterial deodorants (baking soda is a good substitute), and soaps containing antibiotics such as triclosan, which can contribute to breeding resistant bacteria. Exposure to small amounts of pathogenic bacteria is thought to keep the immune system activated.
There is debate over whether high protein or high complex carbohydrate (like whole grains) diets are desirable or not for Candidiasis patients. Protein breakdown can produce ammonia, which in turn creates an environment hospitable to yeast. Complex carbohydrates (starches) can pass far down the gastrointestinal tract before being broken down into glucose and absorbed. Since Candida is thought to sometimes reside and proliferate in the lower gastrointestinal tract, complex carbohydrates could potentially feed Candida there. However complex carbohydrates are necessary for energy and also feed friendly intestinal flora.
Since a major contributing factor to Candida proliferation is usually the elimination of the normal flora, intestinal bacteria must be replaced to help prevent recolonization by Candida. Supplementation with probiotics like Acidophilus bifidus is the usual means of replenishing intestinal flora.
Many therapists recommend avoiding or eliminating yeasted breads and fermented foods from the diet, since a degree of cross-reactivity is suspected. Others argue that eating large quantities of yeast-containing foods may in fact help stimulate antibody production against Candida.
|

